Effective ventilation for mitigating risk in a dental treatment room

Covid-19 restrictions have changed the way many businesses operate throughout New Zealand, and dental practices are no exception to this. While oral health is deemed an essential service and practitioners have a duty of care to support their patients during this time, it is important that steps are taken to protect both staff and patients from the virus. In this article, we discuss how the risk of transmitting Covid-19 within a dental practice can be mitigated by ensuring there is effective ventilation in the treatment rooms to limit exposure during aerosol-generating procedures (AGPs) and isolate high-risk patients.
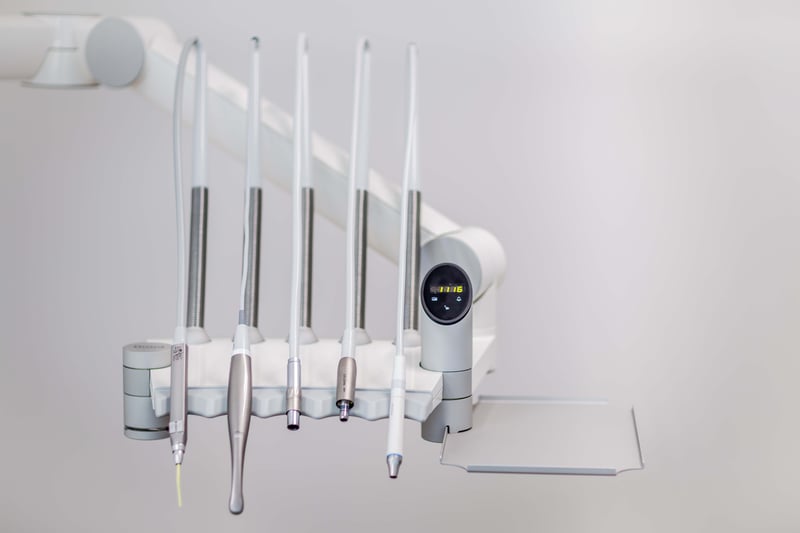
Industry-specific operational conditions have been provided throughout New Zealand to limit the risk of transmission throughout the country. Due to the close-contact nature of the job, dentists are at high risk of occupational exposure to several types of microorganisms, aerosol particles, and droplets that live in patients' saliva and blood and on contaminated instruments, which can be directly responsible for transmitting infectious diseases, including Covid-19.
Therefore, within a dental practice the stipulated guidelines include triaging patients over the phone, when patients can be seen, what type of care can be provided, and minimum room and PPE requirements. As the government's Covid-19 protocols change, so do the conditions required for business operation. For example, under Alert Level 4, it is advised that you only provide urgent or emergency care for your patients, whereas under Alert Level 3, you're able to implement a balance between patients' access to care and protecting public safety by limiting the opportunities for further community spread.
Controls for aerosol-generating procedures
One of the key identified risks of potential virus transmission within a dental practice is through AGPs, such as when rotary handpieces are used. These can promote the generation of small particles (<5 µm) that remain suspended in the air for longer periods than larger particles and can be inhaled, resulting in a risk of airborne transmission.
To combat this it is recommended to avoid AGPs where possible, which includes the use of ultrasonic and sonic scalers, triplex syringe, air-abrasion and air-polishing. It's important to note that all rotary handpieces generate aerosols, regardless of whether the motor is electric or air-driven, both with or without water. This requirement is due to the prolonged nature of such procedures and the close proximity of the operator.
However, in many cases, AGPs are required, therefore it's critical that mitigating measures and airborne precautions are also implemented for patients deemed to be of medium or high risk (standard infection control precautions are required for patients in the low-risk category). These include meeting the correct personal protective equipment (PPE) conditions, ensuring handpieces are used at a slow speed where possible to minimise the aerosol generated during the procedure and that the treatment room aligns with required conditions of operation. For example, using high volume evacuation systems and dental/rubber dams where possible also helps to reduce the extent of aerosol and splatter. AGPs should only be conducted in a room that has natural (such as a window) or mechanical ventilation.
Another required method used to limit the chance of transmission through AGPs is to implement a stand-down period from the room after the procedure is complete but before it is cleaned. This stand-down time depends on the level of risk the patient is classified at and the air changes per hour (ACH) of the treatment room, as outlined below. ACH is a measure of the air volume added to or removed from a space in one hour, divided by the volume of the space.
Recommended post aerosol-generating procedures stand down time for medium - high-risk patient groups under Covid-19 levels 3 and 4, confirmed by the Dental Council of New Zealand (DCNZ).
As demonstrated in the pragmatic algorithm above, the higher the ACH level your heating, ventilation and air conditioning (HVAC) system is able to provide, the less stand-down time required between patients. This improves the productivity and efficiency of your practice during times where these operating conditions are in place, while still effectively managing the risk of transmission and not compromising the safety of your staff or patients.
Implementing negative air pressure in isolation rooms
For patients that are categorised as high risk, which include confirmed and probable cases of Covid-19, those who are symptomatic or waiting on tests, and many frontline workers, an Airborne Infection Isolation Room (AIIR) is required to be used during dental treatments. These are single-occupancy patient-care rooms, also known as negative pressure isolation rooms, used to isolate persons with a suspected or confirmed airborne infectious disease away from other patients, visitors, and healthcare staff. The environmental factors are controlled to minimise the transmission of infectious agents that are usually passed along from person to person by droplets associated with coughing and other airborne fluids.
According to the Center for Disease Control and Prevention (CDC), to meet the conditions AIIRs should provide:
- Negative pressure in the room, which means that the mechanically exhausted air must exceed the mechanically supplied air. This prevents cross-contamination and the spread of a virus by ensuring that air flows from hallways and corridors under the door gap and into the isolation rooms.
- An air flow rate of 6-12 ACH (6 ACH for existing structures, 12 ACH for new construction or renovation) as criteria for an efficient ventilation system.
- Direct exhaust of air from the room to the outside of the building as the first option, or recirculation of air through a high-efficiency particulate air (HEPA) filter before returning to circulation.

If you are unable to meet these conditions and the patient requires care, it is recommended that you refer them to another location where they can receive this. Therefore to avoid losing patients to other oral healthcare providers, ensuring you are able to meet the Covid-19 alert level requirements is important. Keep in mind that some practices have chosen to update each of their treatment rooms to meet these conditions, while others have opted to upgrade only a select few treatment rooms for medium and high-risk patients for the remainder of the period required.
As dental fitout specialists, Dentec are experienced in providing advice for these conditions and with installing efficient ventilation systems for surgery rooms. The process is typically straightforward therefore can be done relatively inexpensively, however, it's important to keep in mind that the requirements are site-specific. Therefore the process usually involves an on-site survey with a technician to work through factors such as the current air conditioning equipment airflows, extraction systems and to locate duct routes.